The PartoMa Project - Co-creating reproductive and newborn health

About the PartoMa Project
The PartoMa project works closely with health providers and pregnant women in busy, low-resource maternity units to co-create interventions for safe and respectful care. Thereby, the PartoMa project responds to gaps in clinical management, which are partly caused by lack of underlying evidence and partly by lack of translation between established medical evidence and clinical practice. In other words, we work on:
- Identifying and filling central gaps in our physiological understanding of pregnancy and childbirth.
- Generating in-depth contextual knowledge on the status and underlying drivers of current childbirth care in busy, low-resource settings.
- Strengthening the translation of current medical knowledge to improve births for mothers and babies where most needed.
Moreover, we aim for the PartoMa research to assist in improving gender equality in health research and decolonize global health agendas (read more).
Since 2014, this has led to co-creation and implementation of integrated, simple and locally achievable clinical guidelines for childbirth care and associated training. Our pilot intervention study from Zanzibar, Tanzania suggested significant improvements in quality of care and survival during birth. Since then, we have commenced bigger scale-up projects in Dar es Salaam, Tanzania, Northern Tanzania and Ethiopia. Furthermore, a major new PartoMa branch is our Co-Creating Antenatal Care (CC-ANC) project. CC-ANC moves PartoMa from childbirth to a broader focus on reproductive health and rights, from a positive pregnancy test till after birth.
In particular, the PartoMa project focuses on childbirth care in urban, low-resource settings. In 2030, the majority of the world’s births occur in urban areas, and a growing ‘urban disadvantage' is reported in several low- and middle-income countries, with poorer outcomes in cities. Though still scarcely researched, these adverse outcomes appear mainly due to urban poverty, lack of basic infrastructure and over-congested health facilities - factors which may all worsen dramatically by the effects of climate changes.
Check out this 2-minutes video update of the PartoMa childbirth intervention in Dar es Salaam, Tanzania:
The PartoMa Birth studies: Co-creating better births

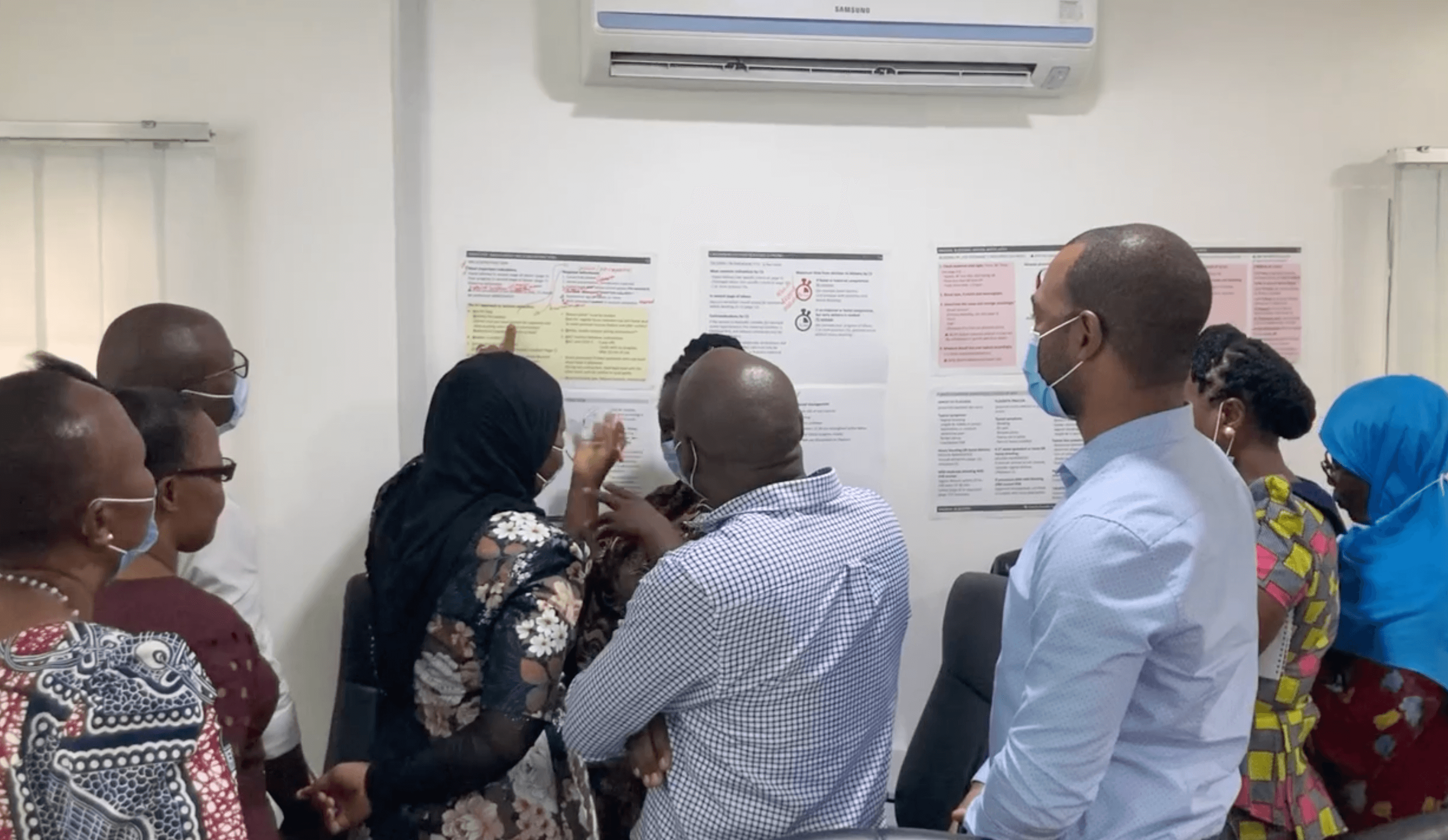
Since 2014, the PartoMa project has developed and implemented simple and locally achievable clinical guidelines and associated training for midwives and doctors in low-resource settings with often alarmingly high numbers of labouring women per birth attendant. As these clinical realities make it practically impossible to adhere to international clinical guidelines, the maternal health staff often use no guidelines or desperately try to work with poorly fitting guidelines. In these settings, there is an urgent need for context-adapted clinical guidance to assist the overwhelmed birth attendants (read more).
The initial PartoMa pilot intervention study in Zanzibar’s tertiary hospital (2014-2018) revealed how simple, locally-tailored guidelines and training could assist birth attendants in delivering more timely and safe care to women giving birth. The results were encouraging with significantly improved survival during birth (read more). Moreover, the project was well-received by Zanzibari health providers who travelled, and are still travelling, long distances to attend the monthly PartoMa training seminars.
In 2019, the PartoMa team initiated a 5-year scale-up research project in Tanzania, with Danida Fellowship Centre (Ministry of Foreign Affairs, Denmark) as the main donor. This PartoMa Scale-Up Project aims to investigate whether the PartoMa pilot intervention from Zanzibar can be modified and scaled to other busy, low-resource maternity units. The intervention is carried out in five urban maternity units in Dar es Salaam who receive the PartoMa intervention as three clusters with 3-month intervals. The first publication on the intervention has now been submitted for publication and more papers will be published in 2023-2024. (read more).
Furthermore, exciting pilot studies have commenced in Northern Tanzania and Ethiopia to assess effects of combining the locally adapted PartoMa guidelines and training with the Laerdal’s MOYO device for monitoring the baby’s heart beat.
The PartoMa Pregnancy study: Co-creating antenatal care

In January 2023, the PartoMa research team received its second major research grant from Danida Fellowship Centre allowing us to move from intrapartum to antenatal care. This new grant supports 5 years of research to explore the reality of health providers and pregnant women and improve quality of care in overburdened urban health facilities in Sub-Saharan Africa. PartoMa’s co-creation and implementation research will now include the entire course of pregnancy - from a positive pregnancy state till after birth.
In Dar es Salaam, Tanzania, one of the world’s fastest growing cities, it now appears more risky for a woman and her baby to undergo pregnancy and birth than in Tanzania’s rural settings. This increasing urban disadvantage is also reported in other resource-constrained cities. Simultaneously, the world’s proportion of births occurring in cities is increasing rapidly while, at the same time, being exposed to the most severe consequences of climate change. In our new Co-Creating Antenatal Care study in Dar es Salaam (the CC-ANC study), the aim is to assess the underlying drivers of risks during pregnancy in the nexus between urbanization and climate change, and to co-create guiding tools to assist both urban pregnant women and their health providers to jointly achieve respectful and safe reproductive health.
With the new CC-ANC study, the team aims to empower pregnant women, their families and their health providers with integrated knowledge and skills related to surveillance, prevention and treatment during pregnancy. For instance, this will include a focus on early pregnancy complications, hypertension and pre-eclampsia, lifestyle and metabolic diseases during pregnancy, bleeding in late pregnancy, birth planning and future contraception counselling.
The PartoMa context studies: Understanding reproductive and newborn health in urban Tanzania

In 2030, the majority of the world’s births occur in urban areas, and a growing ‘urban disadvantage' is suggested in several low- and middle-income countries, with poorer outcomes in cities during pregnancy and childbirth. While literature is scarce, this appears mainly due to urban poverty, lack of basic infrastructure and over-congested health facilities - factors which may all worsen by the consequences of present and future climate changes.
Tanzania exemplifies the dire statistics of urban maternal health: The national incidence of hospital-based neonatal deaths has stagnated since 2006 and neonatal deaths are now significantly higher in Tanzania's urban than in rural areas. This is despite urban rates of facility births above 90%. More specifically, Tanzania’s largest city, Dar es Salaam, the world’s second fastest growing metropole, comprises a particularly high-burden setting with maternal and perinatal mortality considerably higher compared to other regions of the country. At the same time, while healthcare and education systems work beyond capacity, climate-related challenges are intensifying in the city - this causes droughts with intense water rationing for months at a time and extreme heat.
To understand how broader contexts affect care provision, and to inform our co-creation process in Dar es Salaam, we conducted a major mixed-methods in-depth assessment of the status and underlying causes for the quality of childbirth care in the five busiest maternity units of the city. We expect all related papers to be published in 2023-2024. Furthermore, as part of the CC-ANC study, additional mixed-methods studies will be conducted in the coming years on the contextual and health systems factors, including urbanization, climate change, and gender, that enable or hinder adequate care throughout pregnancy.
As called for at the global stage, such new understanding of underlying causes and implementation strategies are needed to accelerate progress in maternal health for women living in urban areas (read more).
The ProLabour initiative: Prolonged labour and overmedicalization during birth
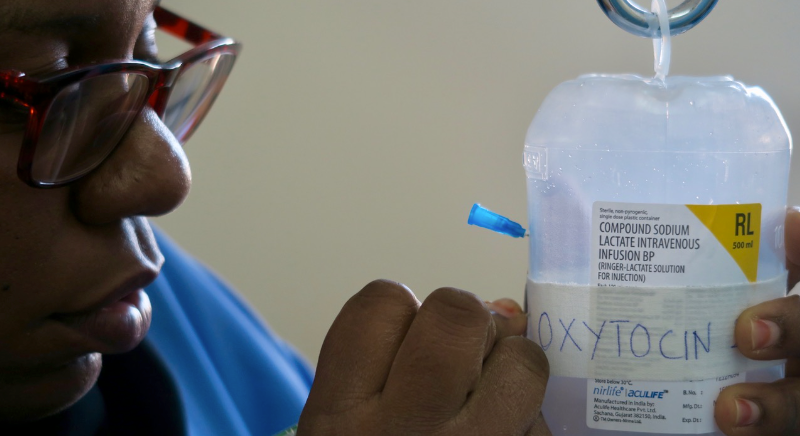
Globally, research indicates alarming high levels of using synthetic oxytocin and caesarean sections to treat prolonged labour, even when labour progress is in fact normal. Both prolonged labour and over-medicalization contribute to distress in unborn babies and mothers, leading to increased risks of disabilities and death. This pattern has been observed as a central and highly concerning issue in our ongoing PartoMa work.
We are currently working on unfolding this major challenge within women’s health in low- and middle-income countries through systematic reviews (read more) and through our situational analyses and intervention work in Tanzania. In high-income countries, a similar trend with an increasing occurrence of over-medicalization of prolonged labour has been reported. For instance, oxytocin for labour augmentation is registered as one of 12 medications on the US’ Institute for Safe Medication Practices’ list of high-alert medications, and incautious use played a central role in 71% of Swedish malpractice cases related to birth asphyxia.
We hope that the next step for the PartoMa team will materialize as a larger research project on how to reach best possible clinical management of prolonged labour. Interestingly, studies from basic and applied sciences suggest bicarbonate (i.e. baking soda) to be safe, low-cost and potentially effective in treating prolonged labour, but more research is needed (read more).
Scientific publications
Kujabi ML, Housseine N, Kabanda I, Msumi R, Maembe L, Sangalala M, Hudson M, Hansen S, Macha A, Sequeira D'mello B, Meyrowitsch DW, Konradsen F, Jensen AK, Hussein K, Maaløe N, van den Akker T. Timing of cesarean section for prolonged labor in urban Tanzania: A criterion-based audit. AJOG Glob Rep. 2024 Oct 10;4(4):100404. doi: 10.1016/j.xagr.2024.100404. PMID: 39583576; PMCID: PMC11582455.
Osaki H, Skovdal M, Sørensen JB, Maaløe N, Housseine N, Dmello BS, Mbekenga C. The Dilemmas and Opportunities of Co-Creating Health Interventions to Fit Local Contexts: An Ethnographic Study on the Adaptation of Clinical Guidelines in Tanzania. Health Expect. 2024 Oct;27(5):e70073. doi: 10.1111/hex.70073. PMID: 39445810; PMCID: PMC11500208.
Sequeira D'mello B, Housseine N, Kidanto HL, Maaløe N, van Roosmalen J, Meyrowitsch DW, van den Akker T, Muniro Z, Polin E, Ambokile N, Festo C, Sørensen JB, Sando D. 'I am happy to be listened to': co-creation of a simple tool to measure women's experiences of respectful maternity care in urban Tanzania. Glob Health Action. 2024 Dec 31;17(1):2403972. doi: 10.1080/16549716.2024.2403972. Epub 2024 Sep 24. PMID: 39314117; PMCID: PMC11423523.
Kujabi ML, Maembe L, Nkungu D, Maaløe N, D'mello BS, van Roosmalen J, van den Akker T, Konradsen F, Hussein K, Pallangyo E, Skovdal M, Sørensen JB. Temporalities of oxytocin for labour augmentation: a mixed-methods study of time factors shaping labour practices in a busy maternity unit in Tanzania. BMC Pregnancy Childbirth. 2024 Aug 29;24(1):563. doi: 10.1186/s12884-024-06717-3. PMID: 39210352; PMCID: PMC11363361.
Kujabi ML, Housseine N, Kabanda I, Msumi R, Maembe L, Sangalala M, Hudson M, Hansen S, Macha A, D'mello BS, Meyrowitsch DW, Konradsen F, Jensen AK, Hussein K, Maaløe N, van den Akker T. Timing of cesarean section for prolonged labor in urban Tanzania: A criterion-based audit. AJOG Global Reports, Volume 4, Issue 4 (2024).
Bakker W, Sandberg EM, Keetels S, Schoones JW, Kujabi ML, Maaløe N, Maswime S, van den Akker T. Inconsistent definitions of prolonged labor in international literature: a scoping review. AJOG Global Reports, Vol. 4, Issue 3 (2024).
Sequeira Dmello, B., John, T.W., Housseine, N. et al. Incidence and determinants of perinatal mortality in five urban hospitals in Dar es Salaam, Tanzania: a cohort study with an embedded case–control analysis. BMC Pregnancy Childbirth 24, 62 (2024).
Osaki H, Sørensen JB, Maaløe N, Mbekenga C, Skovdal M. "It is because the treatment of this lady is a cascade”: Accumulation of delays and the occurrence of obstetric emergencies in an urban maternity unit in Tanzania. Midwifery Vol 130, 2024, 103926, ScienceDirect.
Maaløe N, Kujabi ML, Nathan NO, Skovdal M, Dmello BS, Wray S, van den Akker T, Housseine N. Inconsistent definitions of labour progress and over-medicalisation cause unnecessary harm during birth. BMJ 2023; 383.
Kujabi ML, Mikkelsen E, Housseine N, Obel J, Sequira D’Mello B, Meyrowitsch D, Hussein K, Schroll JB, Konradsen F, van Roosmalen J, van den Akker T, Maaløe N. Labor augmentation with oxytocin in low- and lower-middle-income countries: a systematic review and meta-analysis. AJOG Global Reports. 2022; 2(4).
Sørensen JB, Housseine N, Maaløe N, Bygbjerg IC , Tersbøl BP and Konradsen F. Scaling up Locally Adapted Clinical Practice Guidelines for Improving Childbirth Care in Tanzania: A Protocol for Programme Theory and Qualitative Methods of the PartoMa Scale-up Study, Global Health Action vol. 15, 2022, issue 1
Maaløe N, Housseine N, Sørensen JB, Obel J, DMello BS and Kujabi ML. Scaling up context-tailored clinical guidelines and training to improve childbirth care in urban, low-resource maternity units in Tanzania: A protocol for a stepped-wedged cluster randomized trial with embedded qualitative and economic analyses (The PartoMa Scale-Up Study), Global Health Action vol. 15, 2022, issue 1
Maaløe N, van Roosmalen J, Dmello BS, Kwast B, van den Akker T, Housseine N, Kujabi ML, Meguid T, Kidanto H. WHO next-generation partograph: revolutionary steps towards individualised labour care?, BJOG 2021
Maaløe N, Marie A, Ørtved R, Sørensen JB, Dmello BS, van ven Akker T, Kujabi ML, Kidanto HL, Meguid T, Bygbjerg IC, van Roosmalen J, Meyrowitsch DW, Housseine N. The injustice of unfit clinical practice guidelines in low-resource realities. Lancet Global Health 2021
Sequeira Dmello B, Sellah Z, Magembe G, Housseine N, Maaløe N, Van Den Akker T, Meyrowitsch DW, Mushi T, Masweko M, Jidayi D, van Roosmalen J, Kidanto HL.Learning from changes concurrent with implementing a complex and dynamic intervention to improve urban maternal and perinatal health in Dar es Salaam, Tanzania, 2011-2019. BMJ Global Health 2020
Housseine N, Punt MC, Mohamed AG, Said SM, Maaløe N, Zuithoff NP, Meguid T, Franx A, Grobbee DE, Browne JL, Rijken MJ. Quality of intrapartum care: direct observations in a low-resource tertiary hospital. Reprod Health 2020.
Dmello BS, Housseine N, van den Akker T, van Roosmalen J, Maaløe N. Impact of COVID-19 on maternal and child health. Lancet Global Health 2020.
Housseine N, Punt MC, Browne JL, Van J, Maaløe N, Meguid T, Theron GB, Franx A, Grobbee DE, Visser GHA, Rijken MJ. Delphi consensus statement on intrapartum fetal monitoring in resource settings. Int J Gynaecol Obstet. 2019. 146(1):8-16.
Maaløe N, Meguid T, Housseine N, Tersbøl BP, Nielsen KK, Bygbjerg IC, van Roosmalen J. Local adaption of intrapartum clinical guidelines, United Republic of Tanzania. Bull World Health Organ 2019; 97:365–370.
Housseine N, Punt MC, Browne JL, Meguid T, Klipstein-Grobusch K, Kwast BE, Franx A, Grobbee DE, Rijken MJ. Strategies for intrapartum foetal surveillance in low- and middle-income countries: A systematic review. PLoS One 2018; 13: e0206295.
Maaløe N, Andersen CB, Housseine N, Meguid T, Bygbjerg IC, van Roosmalen JJM. Effect of locally-tailored clinical guidelines on intrapartum management of severe hypertensive disorders at Zanzibar’s tertiary hospital (The PartoMa study). Int J Gynecol Obstet 2018. DOI:10.1002/ijgo.12692.
Maaløe N, Housseine N, Meguid T, Nielsen BB, Jensen AKG, Khamis RS, et al. Effect of locally-tailored labour management guidelines on intrahospital stillbirths and birth asphyxia at the referral hospital of Zanzibar: A quasi-experimental pre-post-study (The PartoMa study). BJOG. 2017;125(2):235–45.
Maaløe N, Housseine N, van Roosmalen J, Bygbjerg IC, Tersbøl BP, Khamis RS, et al. Labour management guidelines for a Tanzanian referral hospital: The participatory development process and birth attendants’ perceptions. BMC Pregnancy Childbirth. 2017;17(175).
Maaløe N, Housseine N, Bygbjerg IC, Meguid T, Khamis RS, Mohamed AG, et al. Stillbirths and quality of care during labour at the low resource referral hospital of Zanzibar: a case-control study. BMC Pregnancy Childbirth. 2016;16 (351).
PhD studies nested within PartoMa
Monica L. Kujabi, PhD student 2021-2024
Labour progression in urban resource-constrained maternity units and beyond: An appeal for change
Nanna Maaløe, PhD student 2014-2018
Assisting Birth Attendant in Providing Acceptable Care under Unacceptable Clinical Realities: The PartoMa Intervention Study at Zanzibar’s Tertiary Hospital
PartoMa guidelines and training material

Dar es Salaam, Tanzania:
- The PartoMa Pocket Guide for Dar es Salaam, version 1.0 (2022)
This version is also being used in Morogoro District of Tanzania.
Sengerema, United Republic of Tanzania:
Zanzibar, United Republic of Tanzania:
PartoMa in the media

- Globally, women in labour are overtreated. The consequences are dire. Article in healthsciences.ku.dk. February 2024.
- Vestimulerende drop er udbredt under fødsler. Men vi ved »alarmerende« lidt om, hvor godt det virker. Article in Information.dk (in Danish), January 2024.
- WHO guidelines are unattainable in poor countries, Videnskab.dk / University of Copenhagen, October 2021
- WHO-guidelines er uopnåelige i fattige lande, Videnskab.dk, October 2021
- Dyster fremskrivning: Flere børn vil dø af coronarestriktioner end det totale antal corona-døde lige nu, Videnskab.dk, august 2020
- Hvad skal der til for at redde liv på en afrikansk fødegang? Det begynder med en læge, der undrer sig – og en simpel idé, Zetland, October 2019
- Fødselslæge vender dyster statistik: »Hver morgen lå der et eller flere døde børn svøbt i deres mødres tørklæder«, Article and podcast in the Danish Medical Bulletin, October 2019
- The PartoMa study and the dangerous coexistence of ‘too much too soon care’ and ‘too little too late care’, Podcast (in Danish) on Stetoskopet, September 2019
- In arme landen loont het om richtlijnen realistisch aan te passen, Medisch contact - a weekly magazine for medical doctors in the Netherlands, May 2019
- Mere sikre fødsler på hospital i Tanzania efter samarbejde med læge fra Hvidovre Hospital, Copenhagen University Hospital Hvidovre, April 2019
- Tanzania redder børns liv i samarbejde med dansk læge, The World’s Best News, February 2019
- Mradi wa PartoMa Waimarisha Huduma Katika Wodi za Mama Wajawazito Zanzibar, World Maelezo latest, July 2018
- Fewer stillbirths at East African hospital following introduction of childbirth guidelines, University of Copenhagen, October 2017
Videos

- The Missing Link between Clinical Guidelines and Clinical Realities: Aligning together. Critical conversation session at the International Maternal Newborn Health Conference (IMNHC), Cape Town, May 2023
- Co-creation with Health Care Providers of Clinical Guidelines for Maternity Care in Dar es Salaam, Tanzania. Presentation at the International Maternal Newborn Health Conference (IMNHC), Cape Town, May 2023
- Update from PartoMa in Dar es Salaam, Tanzania: Clinical guidelines for safe and respectful care during birth. By Nanna Maaløe and Natasha Housseine, November 2022
- The missing link between clinical guidelines and reality: co-creation with birth attendants in Tanzania, Nanna Maaløe’s Nordic Global Health Talk, University of Copenhagen, March 2022
- Maternal Matters - from 3 Ps to 5 Cs, Thomas van den Akker’s inaugural lecture, Vrije Universiteit, Amsterdam, June 2021
- PartoMa seminars – Closing the gap between clinical guidelines and reality, Anthropologist and filmmaker Lara Meguid, March 2018
- Video abstract - Effect of locally tailored labour management guidelines on intrahospital stillbirths and birth asphyxia, British Journal of Obstetrics and Gynaecology, September 2017
Research team
The PartoMa management team
- Dan Wolf Meyrowitsch, MSc, PhD, Associate Professor in Epidemiology, University of Copenhagen
- Nanna Maaløe, MD, PhD, Assistant Professor, Co-founder of PartoMa, University of Copenhagen
- Hussein Lesio Kidanto, MD, MMed ObGyn, PhD, Professor, Aga Khan University, Dar es Salaam Campus
- Natasha Housseine, MD, PhD, Post Doc, Co-founder of PartoMa, Aga Khan University, Dar es Salaam Campus and University of Copenhagen
- Thomas van den Akker, MD, PhD, Professor, Vrije University of Amsterdam
Core senior research team
- Morten Skovdal, MSc, PhD, Associate Professor, University of Copenhagen
- Jane Brandt Sørensen, MA, PhD, Assistant Professor, University of Copenhagen
- Sangeeta Mookherji, MPH, PhD, Assistant Professor, Washington University, USA
- Abera Kenay, MD, PhD, Assistant Professor, Haramaya University, Ethiopia, and Groningen University Medical College, the Netherlands
- Matthew Chersich, Professor, Interlink between climate change and maternal health in Africa, School of Public Health, University of the Witwatersrand, Johannesburg, South Africa
- Ib Christian Bygbjerg, MD, DMSc, Professor, University of Copenhagen
- Jos van Roosmalen, MD, PhD, Professor, Vrije Universiteit Amsterdam
- Andreas Kryger Jensen, MSc, PhD, Associate Professor, University of Copenhagen
- Tarek Meguid, MD, MPhil, MSc, Village Health Works Burundi
- Josephine Obel, MD, MIH, University of Copenhagen
PhD researchers
- Brenda Sequiara DMello, MD, PhD student, Aga Khan University Dar es Salaam / University of Copenhagen
- Fleur Gooren, MD, PhD student, Vrije University of Amsterdam
- Haika Osaki, MPh, PhD student, Aga Khan University Dar es Salaam / University of Copenhagen
- Monica Lauridsen Kujabi, MD, PhD student, University of Copenhagen
- Rashid Saleh Khamis, MD, PhD student, University of Copenhagen
- Thomas John, MD, PhD student, Aga Khan University Dar es Salaam / University of Copenhagen
Support team
- Caroline Clemens Egeland, Special Consultant, University of Copenhagen, Denmark
- Luciana Chamwi, Clinical Officer, Organizer of PartoMa, Aga Khan University, Dar es Salaam Campus, Tanzania
- Morten Mechlenborg Nørulf, Research Communication Specialist, University of Copenhagen, Denmark
- Mwanaarab Sibuma, Research Administrative Officer, Aga Khan University, Dar es Salaam Campus, Tanzania
- Suhaila Salum Yussuf, PartoMa Organiser, Zanzibar Tanzania
- Anna Macha, Medical doctor, Research assistant, Aga Khan University, Dar es Salaam Campus, Tanzania
- Basili Athanasi Joseph, Nurse midwife, Research assistant, Aga Khan University, Dar es Salaam Campus, Tanzania
- Catherine Andrew, Research assistant, Aga Khan University, Dar es Salaam Campus, Tanzania
- Hemed Salehe, Nurse midwife, Research assistant, Aga Khan University, Dar es Salaam Campus, Tanzania
Study advisory board members:
- Lynn Freedman, Professor, Columbia University, United States
- Marian Knight, MPH, PhD, Professor, University of Oxford, UK
- Lenka Benova, MPH, PhD, Associate Professor, Institute of Tropical Medicine in Antwerp and London School of Hygiene and Tropical Medicine
- Anna af Ugglas, Midwife, MPH, Team Lead at Laerdal Global Health for maternal and newborn health education.
- Noah Makula Pauline, PhD, Senior Lecturer, Environmental Assessment and Climate Change Adaptation, University of Dar es Salaam
News from The PartoMa Project
Researchers warn: Denmark will drain the Philippines and India of the health care workers they themselves need
Globally, women in labour are overtreated. The consequences are dire
Urgent action needed to reduce stillborn and newborn deaths in Tanzania
All identifiable people appearing on this website in photos or text have given their oral consent. Photos by Lara Meguid, Tarek Meguid and Nanna Maaløe.
Contact PartoMa
 Dan Meyrowitsch
Dan Meyrowitsch
PI, Professor
University of Copenhagen
Contact
 Nanna Maaløe
Nanna Maaløe
PI, MD, PhD, Associate Professor
University of Copenhagen
Contact
 Hussein Kidanto
Hussein Kidanto
National PI Tanzania, Professor
Aga Khan University
Contact
 Natasha Housseine
Natasha Housseine
Co-PI, MD, PhD, Post Doc
Aga Khan University and University of Copenhagen
Contact
Funding

Main donor of the current PartoMa research is Danida, Ministry of Foreign Affairs of Denmark.
Additional funding has been granted by the Laerdal Foundation, University of Copenhagen, UNICEF and Dr. Thorvald Madsens Legat
